

The NUSS procedure involves surgery to place one or more metal bars in the chest, to elevate the sternum of patients with pectus excavatum. Small incisions are made on either side of the chest through which a small camera and the curved metal bars are inserted. Once in position under the sternum, the bars are flipped and the camera is removed, lifting the chest to correct the pectus deformity. The bars are then secured in place using either sutures or metal stabilisers. You may also have chest drains fitted during surgery, to remove any excess fluid. These will then be removed the following days, once the fluid has drained.
The NUSS procedure is a minimally invasive operation, which uses small incisions causing minimal scarring and reducing the risk of infection. Despite this, it is still major surgery that can be very painful. There are a number of risks and complications that can occur following NUSS surgery, including:
List all to be agreed upon by Simon and Joel
NUSS surgery can be performed at any age but is recommended in late childhood when the sternum is flexible, making it respond better to treatment. As the chest is less flexible the older you are, pectus deformities can be more difficult to correct in adult patients and the risk of experiencing complications increases.
Recovery from the NUSS procedure varies between patients, especially depending on their age. After surgery, patients will spend 2 – 6 days in hospital, where they will receive physiotherapy and support managing their pain levels before being discharged.
In first few the weeks after surgery, patients are encouraged to continue with physiotherapy exercises at home, take short walks (gradually increasing the distance), and slowly decrease the pain killers prescribed. Patients will also need to sleep on their backs in an elevated position.
The Cleveland Clinic estimates it takes about 6 months to fully recover from NUSS surgery, but most people will be able to return to normal activity much sooner (excluding heavy lifting and contact sports). Children should find that they can return to school within one month, whilst adults may take longer to return to work (depending on profession).
Typically, the NUSS bars remain in the chest for a period of 3 years, before they are removed during a second surgical procedure.
Treatment options
Many people with pectus conditions will not experience any physical or psychological symptoms. But for those patients whose physical health or psychological wellbeing are affected, there are ways which symptoms can be treated or managed.
Pectus Matters is dedicated to advocating for a clinical pathway which prioritises early intervention with non-surgical devices. Just like with scoliosis (curvature of the spine), early intervention with non-surgical devices gives patients the best chance of complete correction, minimises the chances of patients developing physical symptoms, and prevents people having to have pectus surgery in the future.
Non surgical
Psychological support
Having a pectus condition can have a big effect on your mental health, regardless of how mild or severe your deformity is. Accessing psychological support, such as Cognitive Behavioural Therapy or Counselling, can be beneficial for patients who are experiencing anxiety, depression, low self-esteem or poor body image because of their pectus condition.
Having a visible chest deformity can have a profound effect on your self-esteem. This can lead to someone having negative thoughts and feelings about themself, the way that they look, and how this reflects on them as a person. Examples of these negative thoughts might include:
-
I am deformed
-
I don’t want people to see me
-
I am abnormal
-
I am weird
-
I look hideous
-
I hate the way that I look
If patients are self-conscious of their chest, they might alter their behaviours to avoid their chest being seen. Examples of this might include:
-
Avoiding sports or swimming
-
Avoiding social events or activities, instead choosing to stay home
-
Avoiding situations where their friends or family might see their chest
-
Feeling forced to wear certain types of clothing to hide the chest
-
Obsessively looking at their chest in the mirror
-
Not wanting to talk about their pectus condition
Most people will experience changes in the shape of their sternum during puberty. Developing a deformity as a teenager – which can already be an emotionally tough time – can have an impact on a young person's body image and self-esteem.
For those whose pectus condition causes them physical symptoms, it is not uncommon for their mental health to suffer; this is especially the case in patients with severe deformities. Experiencing physical symptoms like breathlessness, difficulty swallowing and tachycardia can be scary and managing them day-to-day can have a negative impact on your mental health. Patients might feel anxious and/or depressed as they struggle to manage their physical symptoms: particularly patients who are struggling to access care.
Cognitive Behavioural Therapy and counselling can provide pectus patients with a space to discuss how their condition is affecting them mentally. For some patients, this might be the first time they’ve spoken about pectus deformity, or the only place that they feel comfortable acknowledging the effects it is having on their mental health. Counsellors, psychologists and other mental health professionals provide a listening ear and encourage patients to challenge negative thoughts by setting small tasks or goals to work towards.
Please see some of the resources linked below, for advice and support:
https://www.mind.org.uk/
https://www.youngminds.org.uk
Pectus Matters has trained Mental Health First Aiders who are available to offer support and advice. You can get in touch with us through our contact form or by email at info@pectusmatters.co.uk.
If you or someone you know is having suicidal thoughts or thoughts of harming themself, please contact the Samaritans https://www.samaritans.org/
Physiotherapy
Physiotherapy can be used to assist recovery from surgery, in combination with vacuum bell or bracing, and as an individual therapeutic option. It’s important to note that physio and exercise alone will not reverse a deformity, but it can improve the overall appearance of the chest, strengthen the muscles around the sternum, and improve posture. Building the muscles in the chest can mask the appearance of milder pectus deformities, but it can also make them appear more obvious if it is more severe.
Exercise might be recommended specifically as part of a regimen by a physiotherapist or could just be part of your personal exercise routine. The exercises which are most often recommended to patients with pectus conditions:
Strengthen, stretch and mobilise the muscles in the chest
Build upper body strength
Focus on improving posture
Use deep breathing techniques
Improve general cardiovascular fitness
Check out Hunter Crisp or Pectus PT on Instagram: content creators who have used physiotherapy and exercise to manage their pectus conditions.
Click title to scroll
If you are using a vacuum bell or chest brace, you may be offered physiotherapy to compliment the wearing of non-surgical devices. This could be sessions with a physiotherapist, or a simple list of exercises given to you when you have your device fitted.
If you are having a surgical procedure to correct your pectus condition, you will receive physiotherapy after surgery in the hospital and will be given physio exercises to practice at home once you have been discharged.
Here’s a helpful physio overview for patients having pectus surgery: https://www.southtees.nhs.uk/resources/physiotherapy-for-pectus-repair/
Vacuum bell

A Vacuum Bell device is a non-invasive suction cup, used by patients with pectus excavatum where the sternum sinks in. The vacuum bell sits over the deformed area of the chest and is pumped up and then worn consistently to encourage reshaping over time.
The Vacuum Bell can be prescribed to patients between the ages of 6 and 60, but successful results are seen most frequently in children and teenagers. This is because the sternum is softer and more flexible the younger you are, meaning it is more difficult to achieve perfect results the older the patient is. The device is produced in 5 different sizes with one female version to accommodate the breasts.
To begin with, the device is worn between 1-3 hours per day whilst at rest. Eventually, it is hoped that patients will build up to wearing their vacuum bell for much longer periods, including during sleep. The length of time the device must be used for will depend on how severe your pectus excavatum is and your individual progress. Typically, vacuum bell therapy will last around one year, but patients might be asked to use the device for longer, or to start using it again if their pectus excavatum comes back.
Using the vaccum-bell device can cause dizziness, muscle aches and bruising, as well as general pain and discomfort.
Vacuum Bell’s are medical devices and must be fitted and demonstrated to patients, to ensure safe and proper use. Regardless of whether you get your vacuum bell prescribed through a public health provider (like the NHS) or you purchase it privately, you should seek the advice of a cardiothoracic consultant or orthotist, to ensure that the device is being worn and used correctly.
The device can't be used in patients with;
-
Skeletal conditions such as Osteogenesis Imperfecta (brittle bones) or Osteoporosis
-
Vascular conditions of the central cardiovascular system such as an aneurysm (dilation of the arteries) or as a symptom of Marfan Syndrome, Ehlers-Danlos Syndrome or Loeys-Dietz Syndrome – connective tissue conditions.
-
Blood coagulation disorders such as Thrombopathy or Haemophilia or when taking strong anticoagulants such as Warfarin.
-
If the rib cage is reshaped or supported from within by an implant.
-
When flying or at high altitudes.
-
After diving.
Bracing
Braces are removable devices which are often the first step for treating patients with pectus carinatum or pectus arcuatum. A chest brace might also be recommended for patients with rib flaring (which can occur alongside or because of a pectus condition).
Each model varies in appearance, but all chest braces are made up of a central plate worn over the chest and fitted with straps. The brace applies external pressure to the chest wall, helping to gently reshape the sternum over time.
Bracing tends to be most successful in children and teenagers, as the sternum is softer and more flexible the younger you are. This can mean it is more difficult to achieve perfect results the older the patient is; however, braces are prescribed to adults and can be very successful.
A paediatric consultant, cardiothoracic surgeon, or orthotist will measure and fit you with a chest brace. During your first fitting, the consultant or orthotist may perform some soft tissue massage on the main area of your chest you are looking to target, to soften and flatten the cartilage in the sternum. The chest brace is then fitted so it is ready to be worn.
In the first couple of weeks, you gradually build up the number of hours the brace is worn. After this, the brace is worn for as long as possible during the day and during sleep (up to 23 hours). Typically, chest bracing provides successful results within a year, but this varies and some patients may be required to use a chest brace for a period longer time. Depending on how successful bracing is, you may be able to decrease the number of hours you wear the brace each day.
As a result of wearing a chest brace you might experience skin irritation as well as pain and discomfort. There is a risk of overcorrection of the deformity through chest bracing, this can be avoided by....
Surgical
Surgery should always be the last option for correcting pectus deformities.
For patients with pectus conditions that cause them severe physiological and/or psychological symptoms, surgery may be the only option to help them improve their physical health and mental wellbeing.
Below are some of the different surgical procedures being used to treat pectus conditions. All of these procedures are considered major surgery and come with a number of possible risks and complications that should be considered very carefully before consenting.
Nuss procedure

Ravitch
The Ravitch procedure is a surgical method used to correct pectus excavatum, carinatum and arcuatum.
During the Ravitch procedure, the surgeon will make a large incision (vertically or horizontally) across the chest and remove cartilage, before manually reshaping the sternum. Once the sternum is reshaped, a metal bar, plate or mesh are secured to the sternum to hold the repair in place. You may also have chest drains fitted during surgery, to remove any excess fluid. These will then be removed the following days, once the fluid has drained.
The Ravitch procedure is considered highly invasive surgery, due to the large incision and manual shaping and resetting of the sternum: unlike the NUSS where bars are placed and rotated through small incisions at the side of the chest. Because of this, patients having the Ravitch procedure may expect a longer recovery with an increased risk of infection. List risks and complications associated
The Ravitch procedure can be performed at any age but is recommended in late childhood when the sternum is flexible. As the chest is less flexible the older you are, pectus deformities can be more difficult to correct in adult patients and the risk of experiencing complications increases. Because the Ravitch procedure gives the surgeon the ability to shape the sternum by hand, older patients may find that the Ravitch is the option that provides them with the best chance of a successful correction.
There are a number of other reasons why a cardiothoracic surgeon would choose the Ravitch procedure over the NUSS for a patient. These are:
-
Pectus carinatum
-
A complex or asymmetrical pectus excavatum
-
Previously failed repair
-
Any others
Is recovery any different to NUSS surgery?
If the surgeon uses a bar as the support mechanism, this will need to be removed in the future during a second surgery. If the surgeon uses a plate or mesh, this will not need to be removed.
Pectus up
Pectus Up is a relatively new type of surgery that can be to correct asymmetrical pectus deformities, sternal rotation, or following cardiac surgery or unsuccessful NUSS or Ravitch surgery.
The Pectus Up method involves the placement of a plate and screw onto the sternum through a small, central incision in the chest. Once in place, the screw mechanism is turned to lift the sternum and provide correction. Unlike the NUSS procedure (where bars are removed after 2-3 years), the plate used in Pectus Up remains in the chest meaning only one surgery is required.
Like other surgical methods for treating pectus conditions, there are a number of risks and compilations to be aware of if having Pectus Up surgery.
Seroma, allergy, implant displacement or infection.
You can watch short video on the procedure here: https://youtu.be/gRO1s6F_a-A?t=46
Implants
Pectus implants are made to measure silicone implants which fill the space in the chest created by pectus excavatum. Implants are bespoke made to fit each individual patient and can stay in place for life due to their solid composition which does not create capsular contracture. Surgery to fit a pectus implant is a quick procedure, with a short hospital stay and fast recovery. After surgery a compression garment must be worn for up to 6 weeks, to reduce inflammation.
Having a pectus implant can have complications, such as:
-
Haematoma
-
Seroma
-
Infection
-
Displacement of the implant
-
Development of scar tissue
-
Impaired wound healing


The Scottish National Chest Wall Service strongly advocates for increased access to the vacuum bell for pectus patients, believing that early access to non-invasive treatment is what's best for patients.
Frequently asked questions
The decision about which operation you get is made between you and your surgeon.
Your surgeon will recommend one of the available operations based on how they think they can correct your pectus condition and provide you with the best results. If you are funding surgery yourself then all options are available, but if you are having surgery on the NHS (or HSC in Northern Ireland) the options are more restrictive.
For example, patients accepted by the National MDT through NHS England have two options for surgery: the NUSS procedure and the Ravitch procedure. The NUSS procedure is more commonly used as it’s minimally invasive, but a surgeon may choose the Ravitch if you’ve had a previous pectus or cardiac surgery or a severely asymmetrical sternum. By contrast, in Northern Ireland only the Ravitch procedure is commissioned by HSC.
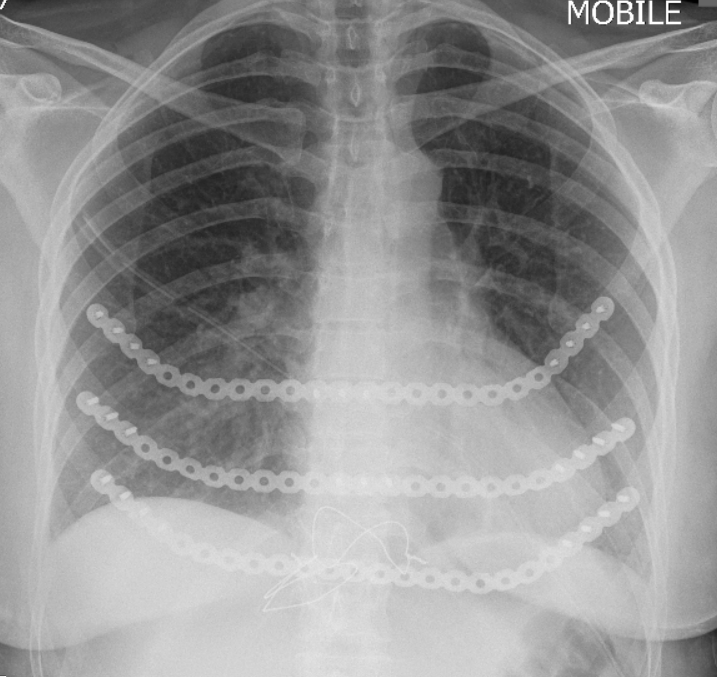
Both the stainless-steel and titanium bars used in pectus surgery are not magnetic, meaning you won’t set off the airport alarms. Despite this, it might be helpful to have a photograph of your chest x-ray on your phone just in case anybody asks about the procedure you’ve had.
Some people choose to create and wear a medic alert bracelet because of their pectus surgery. This is not necessary and is completely personal choice.
A really helpful way to communicate your condition if you are incapacitated and/or unable to answer questions, is to list details of your pectus surgery in the emergency section of your phone. For example, of an iPhone you can create a Medical ID in the Health app that can be viewed by ambulance staff even when your screen is locked.
Yes!
The international guidelines for performing CPR tell every rescuer that you must press on the chest to push it down 5-6cm. This will be more difficult if you have bars or plates in your chest place and therefore more force will be required. If you are having the NUSS procedure and the bars are being removed after 2-3 years, CPR can be performed as normal.
Please note: is an extremely uncommon situation, especially in younger people.
Pain in the mid-upper back is very common after pectus surgery. We think this is because pectus surgery pushes and widens the front of the chest, putting strain on the ligaments between the ribs and the spine. It may also be because after surgery your chest is very stiff, meaning that when you adjust your posture you put strain on the muscles in the thoracic spine.
If you experience this pain after pectus surgery, don’t worry! Most people experience this kind of back pain after pectus surgery as they adjust to their new posture. Careful use of painkillers and physiotherapy should help the muscles in your back adjust to your new posture.
Pectus surgery is major surgery that can be very painful. Aside from painkillers, which will be given to you post-operatively, there are procedures that surgeons can perform to minimize your post-op pain. These procedures happen during surgery when you are asleep to make you more comfortable during your recovery.
Some of these methods are:
-
Cryoanalgesia (nerves in the chest are frozen, numbing them for several months)
-
Thoracic epidural (injecting medication into the area around the spinal cord to reduce pain signals for up to five days)
-
Nerve block infusions (anaesthetic is continuously fed to a group a nerves via a catheter, for a number of days after surgery)
There are pros and cons to the choices between the choices for pain relief after surgery. Ideally patients should be carefully advised of the strategy for pain relief before they give their consent. Clinical teams tend to become very skilled in one method as they know it works for their patients. It is better they use these rather than attempt other strategies that they are not regularly using. There is a need for ongoing research to determine the best methods.
-